What is Asthma?
Asthma is a chronic respiratory condition characterised by both:
- Excessive variation in lung function (more variation and at a greater magnitude than a healthy person would experience), and
- Variable respiratory symptoms, which may include but are not limited to wheezing, shortness of breath, coughing and chest tightness.
(National Asthma Council Australia 2022)
People with asthma are hypersensitive to ‘triggers’ (external stimuli) that may set off symptoms. Triggers commonly include respiratory infections, cigarette smoke, pollen, exercise and dust mites (National Asthma Council Australia 2023).
People with asthma may experience flare-ups when symptoms start or worsen. These require treatment and may become serious medical events (National Asthma Council Australia 2024).
Asthma is considered a spectrum of conditions with several recognised phenotypes that vary in severity (National Asthma Council 2022; Severe Asthma Toolkit 2021).
Asthma is estimated to affect about 2.8 million Australians (11% of the population), with a mortality rate of approximately 1.8 per 100,000 people (AIHW 2024).
Asthma cannot be cured, but if managed properly, most people should be able to enjoy unhindered lives (National Asthma Council Australia 2024).

How Does Asthma Affect the Body?
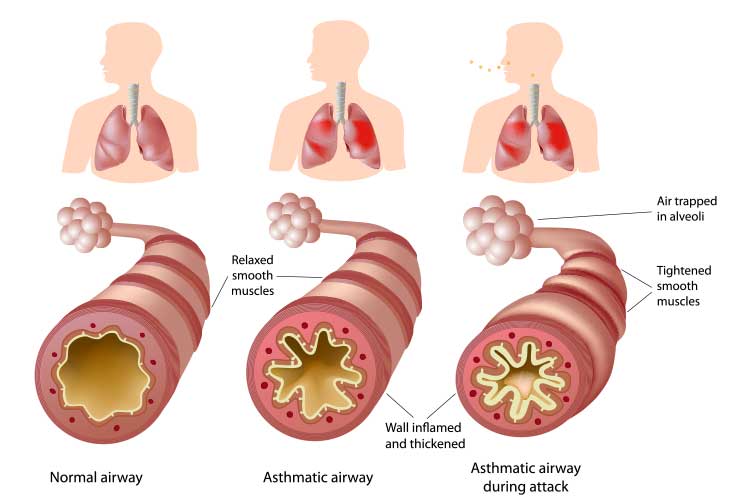
The underlying mechanism of asthma is usually a chronic inflammation of the airways, which is exacerbated by triggers (GINA 2024).
Airway hyperresponsiveness describes the predisposition of the airways to respond to triggers in an exaggerated and reactive way. It involves an increased sensitivity to triggers as well as an excessive constriction of the airways when exposed to them (GINA 2024).
When exposed to triggers, the airways undergo physical changes that result in intermittent airway narrowing. These are:
- Bronchoconstriction: The smooth muscle in the wall of the airways contracts, becoming tighter and narrower. This muscle contracts more easily and strongly in people with asthma.
- Inflammation and swelling of the airway walls, reducing space.
- Excessive mucus production, which blocks the inside of the airways.
(Severe Asthma Toolkit 2022; National Asthma Council 2022)
Diagnosing Asthma
There is no single reliable test to diagnose asthma. Diagnosis is based on the individual’s medical history, physical examination, the consideration of other diagnoses and noting variable airflow limitation. Spirometry is the recommended method for confirming the diagnosis, assessing severity and monitoring asthma (National Asthma Council 2022).
What Causes Asthma?
A combination of genetic and environmental factors is thought to be the cause of asthma (Mayo Clinic 2025).
Risk Factors for Asthma
Risk factors for developing asthma may include:
- Family history of asthma
- Having another atopic condition such as allergic rhinitis (hay fever) or eczema
- Being overweight
- Smoking or second-hand smoking
- Being born prematurely
- Having bronchitis as a child
- Being born at a low birth weight (under 2 kg)
- Exposure to exhaust fumes or pollution
- Exposure to certain chemicals.
(Mayo Clinic 2025; Healthdirect 2024)
Asthma Triggers
Asthma triggers vary from person to person. They may include:
- Pollen
- Dust mites
- Mould spores
- Pet dander
- Respiratory infections (e.g. common cold)
- Physical activity
- Cold air
- Air pollutants (e.g. smoke)
- Medications
- Strong emotions or stress
- Cigarette smoke
- Sulphites and preservatives in foods and beverages
- Gastroesophageal reflux disease.
(Mayo Clinic 2025, National Asthma Council 2022)
Asthma Symptoms
Symptoms vary from person to person. They may be constant or only occur during flare-ups (Mayo Clinic 2025). They may include:
- Shortness of breath
- Chest tightness or pain
- Wheezing or whistling when exhaling
- Coughing or wheezing attacks that are exacerbated by respiratory infections
- Difficulty sleeping due to the above symptoms.
(Mayo Clinic 2025)
Airway Remodelling
Airflow obstruction is usually reversible but some people with asthma may experience airway remodelling - irreversible structural changes to the airways wherein the walls become thicker and the airways become narrower (Severe Asthma Toolkit 2022).
Remodelling is generally thought to be associated with repeated airway tissue destruction and subsequent repair caused by chronic inflammation, but this may not always be the case (Fehrenbach et al. 2017).
Airway remodelling may be related to progressive lung function decline and has been present in cases of fatal asthma (Fehrenbach et al. 2017; Malmström et al. 2017).
For further reading and a more detailed look at developing an asthma management plan, see Auamed’s Article on Recognising and Responding to Acute Asthma.
Test Your Knowledge
Question 1 of 3
Which of the following best defines asthma?
Topics
References
- Australian Institute of Health and Welfare 2024, Chronic Respiratory Conditions: Asthma, Australian Government, viewed 26 March 2025, https://www.aihw.gov.au/reports/chronic-respiratory-conditions/chronic-respiratory-conditions/contents/asthma
- Fehrenbach, H, Wagner, C & Wegmann, M 2017, ‘Airway Remodeling in Asthma: What Really Matters’, Cell and Tissue Research, vol. 367, no. 3, viewed 26 March 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5320023/
- Global Initiative for Asthma 2024, Global Strategy for Asthma Management and Prevention, GINA, viewed 26 March 2025, https://ginasthma.org/2024-report/
- Healthdirect 2024, What Causes Asthma?, Australian Government, viewed 26 March 2025, https://www.healthdirect.gov.au/what-causes-asthma
- Malmström, K, Lohi, J, Sajantila, A, Jahnsen, FL et al. 2017, ‘Immunohistology and Remodeling in Fatal Pediatric and Adolescent Asthma’, vol. 18, no. 94, Respiratory Research, viewed 26 March 2025, https://helda.helsinki.fi//bitstream/handle/10138/190722/Immunohistology_and_remodeling.pdf?sequence=1
- Mayo Clinic 2025, Asthma, Mayo Clinic, viewed 26 March 2025, https://www.mayoclinic.org/diseases-conditions/asthma/symptoms-causes/syc-20369653
- National Asthma Council Australia 2022, Australian Asthma Handbook, National Asthma Council Australia, viewed 26 March 2025, https://www.asthmahandbook.org.au/
- National Asthma Council Australia 2023, What are Asthma Triggers?, National Asthma Council Australia, viewed 26 March 2025, https://www.nationalasthma.org.au/understanding-asthma/what-are-asthma-triggers
- National Asthma Council Australia 2024, What is Asthma?, National Asthma Council Australia, viewed 26 March 2025, https://www.nationalasthma.org.au/understanding-asthma/what-is-asthma
- Severe Asthma Toolkit 2021, Asthma Phenotypes, Severe Asthma Toolkit, viewed 26 March 2025, https://toolkit.severeasthma.org.au/severe-asthma/phenotypes/
- Severe Asthma Toolkit 2022, Asthma Pathophysiology, Severe Asthma Toolkit, viewed 26 March 2025, https://toolkit.severeasthma.org.au/management/asthma-pathophysiology/
 New
New 
