Workers employed by National Disability Insurance Scheme (NDIS) providers, who deliver supports to NDIS participants with an enteral (feeding) tube in place, must be able to provide appropriate support.
Note: This article is intended for NDIS workers and providers. For a more clinically-focused article on enteral feeding, see Caring for Enteral Tubes.
What is Enteral Feeding?
Enteral feeding is the delivery of liquid nutritional support through a tube inserted into the gastrointestinal tract. It is used for people who are unable to meet their nutritional requirements through oral intake. This may be because:
- Their oral intake is inadequate (e.g. poor appetite), or
- They are physically unable to intake orally in a safe way (e.g. dysphagia, reduced level of consciousness).
(DAA 2019)
Enteral feeding may complement oral intake or be used completely in place of oral intake (DAA 2023).
Enteral Feeding Support in the NDIS Practice Standards
Enteral (Naso-Gastric Tube - Jejunum or Duodenum) Feeding and Management is set out in the NDIS Practice Standards under the High Intensity Daily Personal Activities Module.
This Practice Standard aims to ensure that NDIS participants who require enteral feeding and management receive nutrition, fluids and medicines that are appropriate, relevant and proportionate to their individual needs (NDIS 2021).
Under these standards, NDIS providers must meet the following quality indicators:
- Participants are enabled to participate in the assessment and development of an enteral feeding and management plan. This plan identifies possible risks, incidents and emergencies, and what actions need to be taken to manage these situations, including the escalation of care, if necessary. The participant’s health status is reviewed regularly (with their consent).
- Workers providing enteral feeding support are informed by appropriate policies, procedures and training plans.
- Workers providing enteral feeding support have received all necessary training from a qualified health practitioner or another appropriately qualified individual.
(NDIS 2021)
In order to receive enteral feeding support under the NDIS, a participant must have an enteral feeding and management support plan in place. This support plan should be developed in consultation with a health practitioner and may also involve other healthcare professionals such as dieticians, speech therapists or occupational therapists (NDIS 2022).
If the participant is to receive medications through an enteral feeding tube, they should also have a medication plan that outlines this (NDIS 2022).
The participant’s support plan may outline support needs such as:
- The type of enteral feed required
- The feeding delivery mechanism
- Techniques for mealtime assistance
- Stoma care
- Issues to look out for
- Required actions to take in response to risks, incidents and emergencies.
(NDIS 2022)
Enteral Feeding Support Skills Descriptors and Knowledge
The NDIS high intensity support skills descriptors are additional guidance specifically for NDIS workers who are supporting participants with high intensity daily personal activities (HIDPA). Many of these HIDPAs are high-risk and/or intimate care areas that require a high level of care, competency and communication. The high intensity support skills descriptors set out the skills and knowledge required for NDIS workers to effectively and safely support participants with HIDPAs (NDIS 2022).
Skills Required for Enteral Feeding Support
Workers providing enteral feeding support under the NDIS should be able to:
- Understand and follow the participant’s support plan
- Ask the participant about their expectations, capacity and preferences for being involved in the delivery of their care
- Ask the participant about their communication preferences and communicate in their preferred way
- Follow hygiene and infection control principles, including hand hygiene, disinfecting the environment and wearing gloves
- Ensure required equipment and consumables are available and prepared for use
- Support the participant to explore different timings, frequencies, environments, and company for feeding to make the experience more enjoyable
- Provide support in the least intrusive and restrictive way practicable, in alignment with the participant’s daily routine and preferences
- Support the participant to position themselves for feeding and confirm they are ready for their meal
- Set up the water flush, assemble the feed, position the tube and introduce food to the tube
- Monitor the rate, flow and volume of feeding, and adjust this if necessary
- Identify feeding equipment alarms or malfunctions and take appropriate action in response to this
- Identify and immediately escalate issues, such as a broken or displaced feeding tube, or indicators of complications, to an appropriate health practitioner
- Assist the participant in maintaining oral health
- Document required information and observations in the participant’s support plan
- Assist the participant in keeping the stoma healthy and clean
- Work collaboratively with other members of the care team
- Discuss any changes needed to bowel care support with the participant
- Identify, document and report if the participant’s support plan is not meeting their needs
- Support the participant to provide feedback or request changes to their support plan.
Workers supporting a participant with a gastrostomy should be able to:
- Assist the participant in keeping the stoma site healthy and clean
- Recognise and take immediate action in response to a dislodged PEG tube.
Workers supporting a participant to administer medication through an enteral tube should be able to:
- Understand and check the type of medication, dosage, delivery procedure and timing required by referring to the participant’s support plan
- Prepare the medication in accordance with the participant's support plan
- Administer and flush the feeding tube with water in accordance with the participant's support plan
- Prepare and introduce the medication into the feeding tube in accordance with the participant's support plan
- Identify risk indicators such as adverse reactions or overdose and immediately escalate care to an appropriate health practitioner
- Appropriately handle and dispose of sharps and other consumables.
(NDIS 2022)
Knowledge Required for Enteral Feeding Support
NDIS Code of Conduct and Practice Standards
Read: The NDIS Practice Standards Explained
The NDIS Practice Standards establish the benchmark of performance, quality and safety that NDIS providers should meet in their delivery of supports and services (NDIS 2021).
The Standards work alongside the NDIS Code of Conduct to inform NDIS participants about the quality they should be expecting from the supports and services they receive (NDIS 2021).
The NDIS Code of Conduct sets out expectations for the behaviour of both NDIS workers and participants in order to promote safe and ethical service delivery.
The Importance of Good Enteral Feeding Support

Enteral support has a variety of benefits for people who would otherwise be unable to safely or adequately meet their nutritional requirements. These include reversing or preventing malnourishment, improving recovery from illness or surgery, and helping to optimise a person’s quality of life by ensuring they are nutritionally fulfilled, even without oral intake (WACHS 2020).
Therefore, appropriate and competent enteral feeding support is crucial for these participants.
Communication Supports
Participants may have a variety of communication needs and preferences, such as the use of communication aids or devices, or access to resources in another language (NDIS 2022). Remember to individualise communication to ensure each participant’s needs and preferences are met.
For more information on communication supports, see the following Ausmed resources:
Infection Prevention and Control
It’s essential to be aware of and follow infection control principles, including PPE, handwashing and disinfecting (NDIS 2022).
For more information on infection control, see Ausmed’s Training Module on Infection Prevention and Control.
Scope of Practice
Always work within your scope of practice and your role’s responsibilities. Refer to your manager and/or local policies and procedures for more clarity on your specific role and responsibilities if you are unsure.
Also see Ausmed’s Training Module on Scope of Practice: Care Workers.
Types of Enteral Feeding
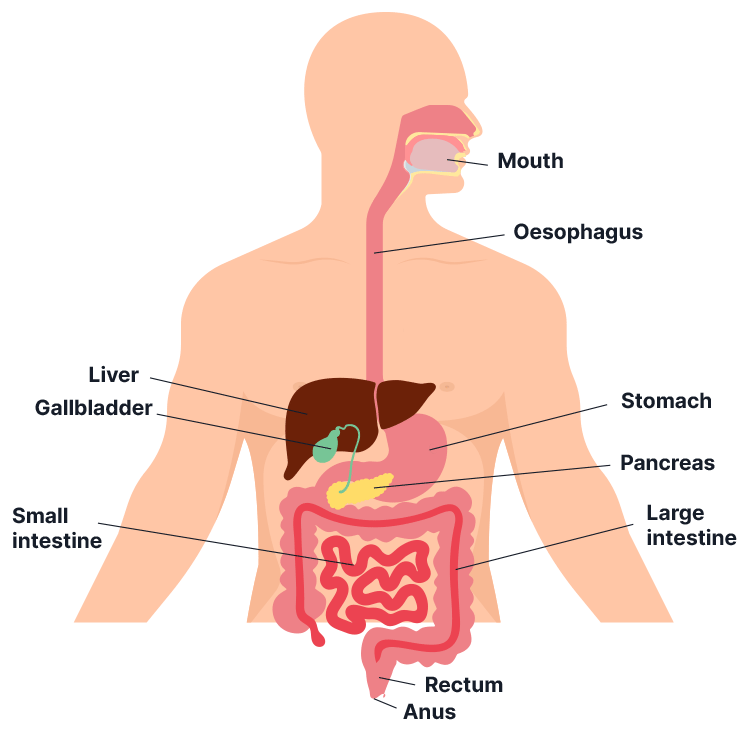
There are three sites on the body where an enteral feeding tube can be inserted, and different route options for each site. The chosen site and route will depend on:
- The intended duration of the nutritional support
- The participant’s condition
- Whether there is any trauma or obstruction that would impede access to a certain site.
(DAA 2018)
The three sites on the body where an enteral feeding tube can be inserted are:
- Gastric (stomach)
- Duodenum (small intestine)
- Jejunum (small intestine).
(WACHS 2020)
The different kinds of tubes that can be used to access each of these sites are:
- Percutaneous endoscopic gastrostomy (PEG) tubes, which are inserted into the stomach via a surgical incision in the abdomen
- Nasogastric (NG) tubes, which are inserted through the nose, down the throat and into the stomach.
(Healthdirect 2024; Cancer Research UK 2024)
As a general rule, NG tubes are usually more appropriate for shorter durations of time, while PEG tubes can stay in situ for longer periods (Ernstmeyer & Christman 2021).
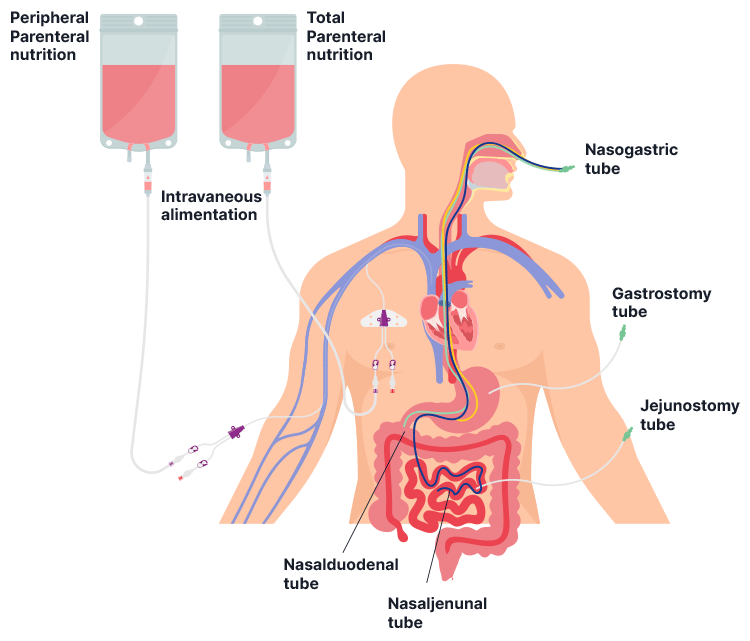
Methods of Tube Feeding
Feed can be administered using one of the following types of equipment:
- A pump is used to administer feed continuously or intermittently
- A gravity drip allows greater quantities of feed to be administered in shorter periods of time
- A syringe is the fastest way of administering feed and allows large amounts of formula to be administered at once.
(RCHM 2024; Ichimaru 2018)
Types of Enteral Feeding Formulas
There are several types of enteral feeding formulas, including:
- Standard (polymeric) formulas: Contain intact proteins, carbohydrates and fats; suitable for people with normal digestion and absorption.
- Semi-elemental formulas: Contain partially hydrolyzed proteins (peptides), partially broken-down fats (medium-chain triglycerides) and simple carbohydrates, making them easier to digest and absorb. These are recommended for individuals with impaired digestion and absorption, such as those with cystic fibrosis or inflammatory bowel disease.
- Elemental formulas: Contain fully hydrolyzed macronutrients, including free amino acids, simple sugars, and minimal fat, making them suitable for people with severe malabsorption, such as those with acute pancreatitis or food allergies. However, these formulas offer limited options and may be challenging for some people to meet protein requirements.
- High-caloric or high-protein formulas: Used for individuals requiring additional energy or protein intake, such as those with high metabolic needs.
- Condition-specific formulas: Tailored to meet the needs of individuals with conditions like liver disease, kidney disease or immune dysfunction.
(McClave et al. 2016; Klimanis 2019; BAPEN 2023a)
The choice of formula depends on factors such as digestive function, caloric requirements, fluid needs and underlying medical conditions.
Equipment for Feeding
- The participant’s feeding regimen
- Gravity feeding set (if using a gravity delivery system)
- Pump feeding delivery set (as required):
- For pre-filled ready-to-hang bags
- Open system for cans, tetras, bottles or modular feed in jugs
- Enteral feeding pump
- Prescribed formula
- Clean container for aspirate
- pH testing strips
- Waterproof sheets
- Disposable cup
- Enteral syringe
- Water for flushing.
(WACHS 2020)
Preparing to Administer Enteral Feeds
- Perform hand hygiene using the 5 moments of hand hygiene.
- Explain the procedure to the participant.
- Confirm the feeding regimen.
- Refer to site-based guidelines for the storage of enteral feeding solutions.
- Document the time and date on the feed container.
- Discard all feeds on their expiry date.
- Duodenal and jejunal feeds need to be administered continuously by pump.
- Remove the formula from refrigeration 30 minutes before use and ensure it is at room temperature before administering.
- Use feeding delivery systems in accordance with the manufacturer’s guidelines.
- Position the participant with the head of the bed elevated 30 to 45° during feeding to reduce the risk of aspiration.
- Ensure the participant stays in this position for at least 30 to 60 minutes after the feed.
(WACHS 2020; RCHM 2024)
Storing Feeds
- Feeds should be stored at room temperature if unopened
- Opened feeds should be kept in the fridge and brought back to room temperature before use
- Dispose of feeds 24 hours after opening
- Store clean enteral feeding equipment at room temperature in a dry container.
(NEMO 2023)
Feeding Pump Alarms, Errors and Maintenance
Alarms and methods for deactivating them will differ depending on the model of device being used. Always refer to the manufacturer’s directions.
If in your scope of practice, you may need to fix blocked or dislodged tubes. Refer to your organisation’s policies and procedures and your position description for more information.
Maintaining Tube Integrity
In order to prevent blockage, tubes should be flushed:
- Before, between and after administering medications
- Every four hours during the day and every eight hours overnight
- Before and after each feed.
(Ernstmeyer & Christman 2021)
Risks and Complications
The potential complications of enteral feeding include:
- Aspiration
- Tube blockage
- Misplaced or dislodged tube
- Infection
- Constipation
- Dehydration
- Delayed gastric emptying
- Diarrhoea
- Fluid overload
- Nausea and vomiting
- Ileus
- Decreased gut mobility
- Abnormal biochemistry
- Allergic reaction
- Mouth discomfort
- Abdominal pain or distension
- Reflux
- Mouth discomfort or infection.
(WACHS 2020; BAPEN 2023b; CDHB 2022)
These complications can cause significant discomfort to participants and may develop into more serious concerns - for example, aspiration can lead to pneumonia (Mcilvoy 2019).
High Risk Indicators
The following signs may be indicative of an issue:
- Coughing (especially a wet cough)
- Vomiting
- Changed bowel habits
- Unplanned weight gain or loss
- Dehydration
- Allergic reaction
- Diarrhoea
- Constipation.
(NDIS 2022)
Oral Health
People receiving enteral nutrition with little or no oral intake are at risk of issues such as dry mouth, oral infection and mouth discomfort. Therefore, maintaining good oral hygiene is essential in minimising the risk of these problems and optimising participants’ comfort (BAPEN 2023b).
Management
You may have specific documentation and reporting responsibilities, such as handover, observations and incident reporting (NDIS 2022). Refer to your organisation’s policies and procedures for further information on what is required.
You should also be aware of the process for requesting a review of a participant’s care (NDIS 2022). Refer to your organisation’s policies and procedures for further information.
When to Escalate Care
A participant should be referred to your manager or an appropriately qualified healthcare practitioner (refer to your organisation’s policies and procedures) if they are experiencing any of the following complications:
- Broken or dislodged feeding tube
- High risk indicators or signs of health-related complications.
(NDIS 2022)
Additional Support
Medication Support
Workers supporting a participant to administer medication through an enteral tube are required to also have knowledge on:
- Methods, equipment and consumables used to administer medication through an enteral tube
- The purpose of the medications being administered to the participant
- Medication storage requirements
- Factors that may affect the administration of medication through an enteral tube
- Signs and symptoms of adverse reactions to medications and dosage errors.
(NDIS 2022)
Gastrostomy Support
Workers supporting a participant with a gastrostomy are required to also have knowledge on:
- How to maintain different types of stomas, including:
- Cleaning the stoma
- Protecting the skin around the stoma site
- Checking and refilling the balloon
- What a healthy stoma should look like
- Signs of an issue at the stoma site, e.g. wetness, infection or inflammation - and what actions are required to manage these
- Their documentation responsibilities.
(NDIS 2022)
Conclusion
NDIS providers should ensure that staff supporting participants with enteral feeding have the skills and knowledge outlined by the Skills Descriptors, and are reviewed annually for competency (NDIS 2022).
Test Your Knowledge
Question 1 of 3
Which one of the following is NOT a key component of an enteral feeding and management support plan?
Topics
Further your knowledge

 Free
Free Free
FreeReferences
- Agency for Clinical Innovation 2024, Home Enteral Nutrition: For Individuals and Their Carers, New South Wales Government, viewed 19 February 2025, https://aci.health.nsw.gov.au/networks/nutrition/resources/home-enteral-for-individuals
- The British Association for Parenteral and Enteral Nutrition 2023a, Choice of Enteral Tube Feed, BAPEN, viewed 20 February 2025, https://www.bapen.org.uk/education/nutrition-support/enteral-nutrition/choice-of-enteral-tube-feed/
- The British Association for Parenteral and Enteral Nutrition 2023b, Management of Enteral Feeding Complications, BAPEN, viewed 19 February 2025, https://www.bapen.org.uk/education/nutrition-support/enteral-nutrition/management-of-enteral-feeding-complications/
- Cancer Research UK 2024, Drip or Tube Feeding, Cancer Research UK, viewed 19 February 2025, https://www.cancerresearchuk.org/about-cancer/coping/physically/diet-problems/managing/drip-or-tube-feeding/types
- Canterbury District Health Board 2022, Enteral Feeding Policy, Health New Zealand, viewed 19 February 2025, https://edu.cdhb.health.nz/Hospitals-Services/Health-Professionals/CDHB-Policies/Clinical-Manual/Documents/Enteral-Feeding%20Policy.pdf
- Dietitians Association of Australia 2019, Nutrition and Hydration Policy Support Handbook For Acute Adult Inpatient Setting, DAA, viewed 19 February 2025, https://member.dietitiansaustralia.org.au/Common/Uploaded%20files/DAA/Resource_Library/2022/Nutrition_and_Hydration_handbook_February_2019_APPROVED.pdf
- Dietitians Association of Australia 2023, Enteral Nutrition, DAA, viewed 19 February 2025, https://dietitiansaustralia.org.au/health-advice/enteral-nutrition
- Ernstmeyer, K & Christman, E 2021, ‘Chapter 17 Enteral Tube Management’, in Nursing Skills, Chippewa Valley Technical College, viewed 19 February 2025, https://www.ncbi.nlm.nih.gov/books/NBK593216/
- Healthdirect 2024, PEG Tube Placement, Australian Government, viewed 19 February 2025, https://www.healthdirect.gov.au/peg-tube-placement
- Ichimaru, S 2018, ‘Methods of Enteral Nutrition Administration in Critically Ill Patients: Continuous, Cyclic, Intermittent, and Bolus Feeding’, NCP, vol. 33, no. 6, viewed 20 February 2025, https://aspenjournals.onlinelibrary.wiley.com/doi/10.1002/ncp.10105
- Klimanis, A 2019, ‘Enteral Nutrition Overview and Formula Selection Considerations’, Dietitians On Demand, 31 August, viewed 20 February 2025, https://dietitiansondemand.com/enteral-nutrition-overview-formula-selection-considerations/
- McClave, SA, Taylor, BE, Martindale, RG 2016, ‘Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient’, JPEN, vol. 40, no. 2, viewed 20 February 2025, https://aspenjournals.onlinelibrary.wiley.com/doi/full/10.1177/0148607115621863
- Mcilvoy, L 2019, ‘Tube Feeding Aspiration’, American Nurse Today, vol. 15, no. 3, viewed 19 February 2025, https://www.myamericannurse.com/tube-feeding-aspiration/
- NDIS Quality and Safeguards Commission 2021, NDIS Practice Standards and Quality Indicators, Australian Government, viewed 19 February 2025, https://www.ndiscommission.gov.au/sites/default/files/2022-02/ndis-practice-standards-and-quality-indicatorsfinal1_1.pdf
- NDIS Quality and Safeguards Commission 2022, NDIS Practice Standards: High Intensity Support Skills Descriptors, Australian Government, viewed 19 February 2025, https://www.ndiscommission.gov.au/sites/default/files/2024-09/High%20Intensity%20support%20skills%20descriptors.pdf
- Nutrition Education Materials Online 2023, What You Need to Know About Tube Feeding at Home, Queensland Government, viewed 20 February 2025, https://www.health.qld.gov.au/__data/assets/pdf_file/0029/1281944/info-tube-feeding-home.pdf
- Queensland Health 2011, Tube Feeding at Home, Queensland Government, viewed 19 February 2025, https://www.yumpu.com/en/document/read/11282788/tube-feeding-at-home-queensland-health
- Queensland Health 2022, Enteral Nutrition Products and Food Supplements, Queensland Government, viewed 19 February 2025, https://www.health.qld.gov.au/__data/assets/pdf_file/0024/443607/enteral-nutrition.pdf
- Royal Children's Hospital Melbourne 2024, Enteral Feeding and Medication Administration, RCHM, viewed 20 February 2025, https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Enteral_feeding_and_medication_administration/#equipment-for-feeding
- Western Australia Country Health Service 2020, Enteral Tubes and Feeding - Adults Clinical Practice Standard, Government of Western Australia, viewed 19 February 2025, https://www.wacountry.health.wa.gov.au/~/media/WACHS/Documents/About-us/Policies/Enteral-Tubes-and-Feeding---Adults-Clinical-Practice-Standard.pdf?thn=0
 New
New 
