Loss of bone density occurs naturally with age, but for the 1.2 million Australians living with osteoporosis (Healthy Bones Australia 2024a), even a small fall or mechanical injury could mean a trip to hospital.
What is Osteoporosis?
The aptly-named osteoporosis (meaning ‘bones with holes’) is a condition causing bones to become more porous due to loss of density (Better Health Channel 2023).
This decreased density means the bones are weaker, thinner and more fragile, which makes them more susceptible to breakage. As a result, the potential for injury - even from minor accidents - is increased (AIHW 2024).
Osteoporosis v Osteopaenia
When bones lose minerals (such as calcium) more quickly than they can be replenished, their density decreases. Peak bone density is reached between the ages of 25 and 30, and after about 50, the body begins to break down more bone than it can rebuild (Better Health Channel 2023; MHA 2024).
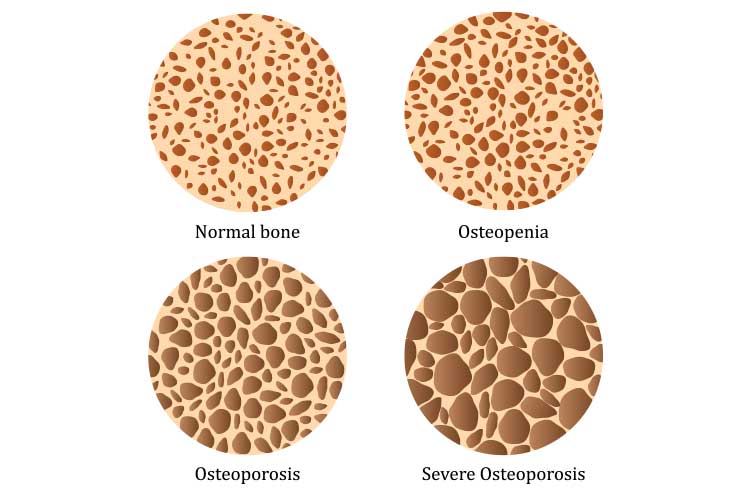
Loss of bone mineral density can be sorted into three categories depending on how far it has progressed.
These three categories are:
- Normal bone density
- Osteopaenia (below average bone density)
- Osteoporosis (significantly below average bone density).
(MHA 2024)
Osteopaenia is a condition in which there has been some loss of bone density, and bones are therefore weaker but not frail enough to be considered osteoporosis (AIHW 2024).
A person who has developed osteopaenia will not necessarily progress to having osteoporosis, but could be at greater risk of doing so (Healthdirect 2024).
How Common is Osteoporosis?
Because osteoporosis often doesn’t present with symptoms, it’s likely to be underdiagnosed, with the exact prevalence is difficult to determine (AIHW 2024).
Osteoporosis is more common in people aged over 50, especially women due to the bone density loss associated with menopause (MHA 2024; Better Health Channel 2024.
Signs and Symptoms of Osteoporosis
Osteoporosis is known as a ‘silent disease’ because there are usually no obvious symptoms until a fracture occurs (Better Health Channel 2023).
For this reason, it’s recommended that any person over 50 who suffers a broken bone from a minor accident or fall should be tested for osteoporosis (Healthy Bones Australia 2023).
The following signs and symptoms may suggest osteoporosis:
- Back pain
- Loss of height
- Stooped posture
- A bone that breaks more easily than expected.
(Mayo Clinic 2024)

Risk Factors for Osteoporosis
There are certain risk factors that can be used to predict the occurrence of osteoporosis.
Naturally, the presence of osteopaenia could suggest progression to osteoporosis in the future.
Other risk factors include:
- Being female, particularly of European or Asian descent
- Having an early menopause (bone health is related to the amount of oestrogen in the body, which decreases after menopause)
- Being of an older age
- A family history of osteoporosis
- Low calcium or vitamin D levels
- Having a small body frame
- Certain medical conditions (such as low hormone levels, malabsorption conditions, thyroid conditions, chronic diseases)
- Taking certain medications (e.g. corticosteroids)
- Lifestyle factors (smoking, lack of physical activity, excessive alcohol intake, being overweight or obese).
(Mayo Clinic 2024; Healthy Bones Australia 2024b; Healthdirect 2023)
Diagnosing Osteoporosis
A bone density test known as the dual-energy x-ray absorptiometry (DXA/DEXA) scan can be used to diagnose osteoporosis.
The scan uses radiation to measure bone tissue in the spine and hip and provides a ‘T-Score’, which categorises the individual’s bone density as either normal, osteopenia or osteoporosis (MHA 2024).
Impacts of Osteoporosis
Osteoporosis can lead to fractures in any bone, but the hip, spine and wrist are the most commonly fractured areas (MHA 2024).
In severe cases of osteoporosis, the bones are so thin that even coughing or bending over is enough to cause a fracture (Mayo Clinic 2024).
The fractures caused by osteoporosis can have a significant impact on the individual’s life, leading to chronic pain, disability, loss of independence or even death in some cases (AIHW 2024).
For this reason, osteoporosis has the potential to be severe or fatal if an accident occurs.
Once an individual has experienced an initial fracture due to osteoporosis, they have a 50% chance of experiencing another fracture (Arthritis & Osteoporosis Tasmania 2022).
This creates a ‘cascade effect’, which means the individual becomes more and more likely to suffer another fracture with each subsequent injury (Arthritis & Osteoporosis Tasmania 2022).
Osteoporosis can also cause the vertebrae to weaken and crumple, leading to spinal injuries without an accident having occurred (Mayo Clinic 2024).
Preventing Osteoporosis
Although the genetic risk factors of osteoporosis cannot be changed, it’s possible for an individual to reduce the possibility of developing osteoporosis by managing aspects of their lifestyle.
It’s important to ensure that the bones are thick and healthy from a young age before density begins to decrease.
The following are crucial to ensuring optimal bone health:
- Maintaining a nutritious diet with adequate calcium
- Getting enough vitamin D
- Exercising regularly
- Only consuming alcohol in moderation
- Refraining from smoking.
(MHA 2024; Healthdirect 2023)

Managing Osteoporosis
There is no cure for osteoporosis, but an individual may be prescribed medication to strengthen their bones and reduce the amount of density lost (Healthdirect 2023).
They may also be advised to make lifestyle changes. However, the most important way to manage osteoporosis is to focus on fall prevention and put measures into place to reduce the risk of having an accident.
This includes reducing tripping hazards around the home, using walking sticks or frames to assist with steadiness and avoiding certain chores or tasks.
After the onset of osteoporosis, it is important to stop the cascade effect from occurring.
Test Your Knowledge
Question 1 of 3
Once an individual has experienced their first fracture from osteoporosis, how likely is it that they will experience another one?
Topics
References
- Arthritis & Osteoporosis Tasmania 2022, Osteoporosis Statistics, Arthritis & Osteoporosis Tasmania, viewed 3 March 2025, https://arthritistas.org.au/osteoporosis/osteoporosis-statistics/
- Australian Institute of Health and Welfare 2024, Osteoporosis and Minimal Trauma Fractures, Australian Government, viewed 28 February 2025, https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/musculoskeletal-conditions/contents/osteoporosis
- Better Health Channel 2023, Osteoporosis, Victoria State Government, viewed 28 February 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/osteoporosis
- Better Health Channel 2024, Menopause and Osteoporosis, Victoria State Government, viewed 3 March 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/menopause-and-osteoporosis
- Healthdirect 2023, Osteoporosis, Australian Government, viewed 3 March 2025, https://www.healthdirect.gov.au/osteoporosis
- Healthdirect 2024, Osteopaenia, Australian Government, viewed 28 February 2025, https://www.healthdirect.gov.au/osteopaenia
- Healthy Bones Australia 2023, Breaking a Bone and Bone Health, Healthy Bones Australia, viewed 3 March 2025, https://healthybonesaustralia.org.au/resource-hub/fact-sheets/breaking-bone/
- Healthy Bones Australia 2024a, About Osteoporosis, Healthy Bones Australia, viewed 28 February 2025, https://healthybonesaustralia.org.au/your-bone-health/about-osteoporosis/
- Healthy Bones Australia 2024b, Risk Factors, Healthy Bones Australia, viewed 3 March 2025, https://healthybonesaustralia.org.au/your-bone-health/risk-factors/
- Mayo Clinic 2024, Osteoporosis, Mayo Clinic, viewed 3 March 2025, https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- Musculoskeletal Health Australia 2024, Understanding Osteoporosis, MHA, viewed 28 February 2025, https://muscha.org/osteoporosis/
 New
New