What is a Peptic Ulcer?
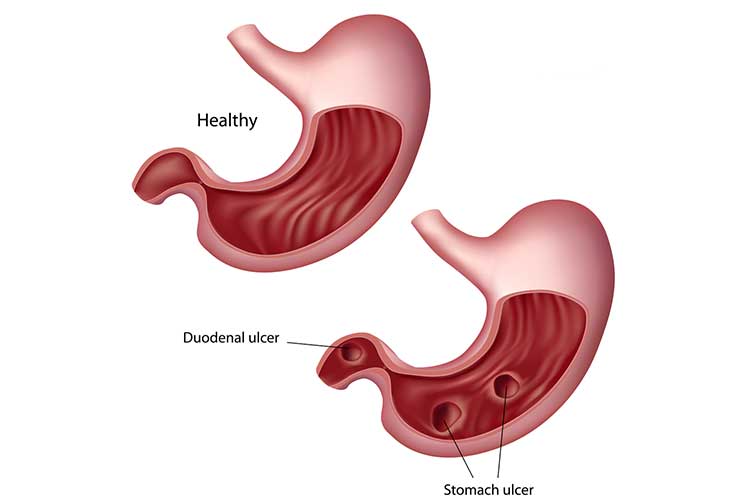
Peptic ulcers occur in the lining of the stomach or on the upper section of the small intestine (duodenum). They can be categorised as either:
- Gastric ulcers: Ulcers that occur on the inside of the stomach
- Duodenal ulcers: Ulcers that occur on the inside of the small intestine.
(Mayo Clinic 2024; Schafer et al. 2021)
Normally, the lining of the stomach and intestines has defences against acid produced by the stomach. However, when something interferes with those defences, the acid may cause damage. A peptic ulcer is a product of this damage; it is an open and inflamed sore (MSD Manual 2023; Mayo Clinic 2024).
Peptic ulcers vary in size, ranging from millimetres to centimetres (Vakil 2023a).
It’s crucial that peptic ulcers are diagnosed and treated early to avoid severe complications (Malik et al. 2023).

Causes of Peptic Ulcers
The most common causes of peptic ulcers are:
- Helicobacter pylori (H. pylori) bacterial infection, which causes approximately 70% to 90% of gastric ulcers and 90% of duodenal ulcers
- Use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin.
(Healthdirect 2023; Malik et al. 2023)
Note that spicy foods and stress do not cause peptic ulcers, but can worsen symptoms (Mayo Clinic 2024).
Symptoms of Peptic Ulcer
Often peptic ulcers will not present with any symptoms (Mayo Clinic 2024).
If symptoms do occur, they most commonly include a burning, gnawing or aching pain in the upper abdomen. The pain often comes and goes in intervals (Vakil 2023a).
Other symptoms include:
- Indigestion (heartburn)
- Nausea and/or vomiting
- Feeling full and bloated, or belching.
(Mayo Clinic 2024; Malik et al. 2023)
Eating food may dull the symptoms of duodenal ulcers but can worsen the symptoms of gastric ulcers (Vakil 2023a).
What are the Complications of Peptic Ulcers?
Peptic ulcers may lead to the following:
- Gastrointestinal haemorrhage, which may lead to:
- Passing bloody stools or black, tarry stools
- Vomiting blood, or blood that looks like ground coffee
- Perforation through the wall of the stomach or small intestine, which can cause severe infection and pain
- Penetration through the muscular wall of the stomach or duodenum into the liver, pancreas or another organ
- Gastrointestinal obstruction
- Stomach cancer risk increases three to six-fold in patients with H. pylori-related ulcers.
(MSD Manual 2023; Vakil 2023a)
Risk Factors for Peptic Ulcers
Peptic ulcers can affect people of any age. However, they mostly occur in people over 60 and males are more commonly affected than females (NHS 2022).
Smoking is still considered a risk factor for the development of ulcers and the complications they cause. Additionally, smoking is known to impede healing and increase the chance of recurrence (Vakil 2023a).
Other risk factors include:
- Family history of peptic ulcers
- Taking certain medications, including corticosteroids and bisphosphonates
- Illnesses causing a hypersecretory environment, such as cystic fibrosis.
(Malik et al. 2023)
Diagnosing Peptic Ulcers
A general practitioner may suggest an examination if a patient has stomach pain characteristic of ulcers.
Tests may need to be performed:
- If symptoms do not resolve following multiple weeks of treatment
- When symptoms first appear in someone over the age of 45
- If a person is presenting with other symptoms such as weight loss.
(Vakil 2023a)
Diagnostic methods may include:
- Endoscopy
- Biopsy if an ulcer is found during the endoscopy
- C14 breath test to check for H. pylori.
(Better Health Channel 2023)
Treating Peptic Ulcers
Treatment of gastric and duodenal ulcers involves removing the cause, which may require:
- Antibiotics in the case of H. pylori infection
- Acid-suppressing medications (e.g. proton pump inhibitors)
- Antacids.
(MSD Manual 2023)
Note that even after successful treatment, approximately 60% of ulcers will recur (Malik et al. 2023). However, eradicating H. pylori significantly reduces this risk of recurrence (Vakil 2023b).
Preventing Peptic Ulcers
- Protect from infection through good hygiene practices
- Avoid overusing NSAIDs - if painkillers are required, they should be taken with meals.
(Malik et al. 2023; Mayo Clinic 2022)

Test Your Knowledge
Question 1 of 3
True or false: Peptic ulcers mostly occur in people under 60 years of age.
Topics
References
- Better Health Channel 2023, Stomach Ulcer, Victoria State Government, viewed 11 November 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/stomach-ulcer
- Healthdirect 2023, Stomach Ulcers, Australian Government, viewed 11 November 2024, https://www.healthdirect.gov.au/stomach-ulcers
- Malik, TF, Gnanapandithan, K & Singh, K 2023, ‘Peptic Ulcer Disease’, StatPearls, viewed 11 November 2024, https://www.ncbi.nlm.nih.gov/books/NBK534792/
- Mayo Clinic 2024, Peptic Ulcer, Mayo Clinic, viewed 11 November 2024, https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/symptoms-causes/syc-20354223
- MSD Manual 2023, Quick Facts: Peptic Ulcer Disease, MSD Manual Consumer Version, viewed 11 November 2024, https://www.msdmanuals.com/en-au/home/quick-facts-digestive-disorders/gastritis-and-peptic-ulcer-disease/peptic-ulcer-disease
- National Health Service 2022, Stomach Ulcer, NHS, viewed 11 November 2024, https://www.nhs.uk/conditions/stomach-ulcer/
- Schafer, TW, Caufield, SP & DeBanto, J 2021, Peptic Ulcer Disease, American College of Gastroenterology, viewed 11 November 2024, https://gi.org/topics/peptic-ulcer-disease/
- Vakil, N 2023a, Peptic Ulcer Disease, MSD Manual Consumer Version, viewed 11 November 2024, https://www.msdmanuals.com/en-au/home/digestive-disorders/gastritis-and-peptic-ulcer-disease/peptic-ulcer-disease
- Vakil, N 2023b, Peptic Ulcer Disease, MSD Manual Professional Version, viewed 12 November 2024, https://www.msdmanuals.com/professional/gastrointestinal-disorders/gastritis-and-peptic-ulcer-disease/peptic-ulcer-disease
 New
New