Aged care governance in Australia has undergone significant reform following the Royal Commission into Aged Care Quality and Safety. One of the key outcomes of these reforms is the Responsible Persons Duty, introduced under the Aged Care Act 2024. This duty applies to directors, senior executives, and managers of aged care providers. It establishes legal obligations to exercise due diligence in ensuring care quality, risk management, and compliance with regulatory requirements.
Directors and senior leaders must take active steps to ensure their organisations meet the Provider Duty, which requires that aged care services do not cause harm to individuals and uphold the highest standards of safety and quality.
This article explores:
- Governance best practices
- Who the Responsible Persons Duty applies to
- Key regulatory requirements to stay across
- The role of risk management
- How resourcing and responsiveness impact compliance
1. Governance Best Practices
Governance in aged care requires a strong commitment to leadership, accountability, and ethical decision-making. The following best practices help directors and executives ensure compliance, risk management, and quality improvement:
- Transparency and accountability - Boards must promote clear decision-making, ethical leadership, and public accountability.
- Risk-based thinking - Directors should proactively assess clinical, financial, and operational risks using a structured risk management framework.
- Client-centred governance - Decision-making should prioritise the wellbeing, dignity, and rights of aged care residents, aligning policies with the Statement of Rights.
- Compliance and legal oversight - Directors must regularly review governance policies to ensure adherence to aged care legislation, accreditation standards, and workforce requirements.
- Continuous improvement - Providers should regularly train staff, review consumer feedback, and implement quality assurance measures to enhance aged care services.
For more insights on governance best practices, visit:
- Governance in Aged Care Course (Australian Institute of Company Directors)
- Governance and Leadership in Aged Care (Ausmed)

2. Who Does this Duty Apply To?
The Responsible Persons Duty applies to all individuals involved in the governance of an aged care provider, including:
- Directors - Board members who provide strategic oversight and decision-making.
- Senior Executives - Leaders responsible for operational governance and implementation.
- Managers - Individuals overseeing specific service areas or compliance functions.
Even though frontline care workers are not directly responsible, directors and senior managers must ensure that systems, training, and policies are in place to enable safe and high-quality care.
Failure to meet this duty can result in:
- Significant financial penalties for breaches. Failure to comply with governance obligations can result in severe penalties. Under the Aged Care Act 2024, aged care providers and directors may face:
- Fines of up to $55,000 for breaches of governance and quality standards.
- Revocation of accreditation and funding for persistent non-compliance.
- Criminal prosecution in cases of severe neglect or failure to report abuse (this will be removed for individual directors in place of serious civil penalties)
- Personal liability for directors who fail to exercise due diligence in governance.
- Regulatory intervention by the Aged Care Quality and Safety Commission (ACQSC).
- Potential bans from serving in leadership roles in aged care.
For an overview of compliance penalties, visit the Aged Care Quality and Safety Commission’s Compliance and Enforcement.
With increased scrutiny and higher community expectations, responsible persons must ensure strong oversight, proactive risk management, and a culture of continuous improvement in aged care governance.
3. Regulatory Knowledge: Understanding Compliance Obligations
Directors must have a clear understanding of and keep up to date with the legal and regulatory framework governing aged care services.
Auditors will assess:
- How well the board understands its obligations.
- Whether directors receive regular training and updates.
- How compliance frameworks reflect evolving regulatory requirements.
The key frameworks are summarised below.
Aged Care Act 2024
Refer to the Aged Care Act 2024 for the full legislative details. In summary:
- Outlines the legal responsibilities of aged care providers and their leaders.
- Establishes the Provider Duty, which requires providers to ensure their conduct does not cause adverse effects on individuals’ health and safety.
Code of Conduct for Aged Care
The Code of Conduct is published by the Aged Care Quality and Safety Commission. For complete guidance, refer to the official Code of Conduct or this Ausmed article or training module. In summary:
- Applies to providers, aged care workers, volunteers and directors.
- Requires leaders to act with integrity, honesty, and transparency.
- Mandates proactive action to address safety risks and ethical concerns.
Aged Care Quality Standards (Effective July 2025)
For detailed information and the strengthened Standards, refer to the Commission’s website. In summary:
- Establishes minimum service standards that providers must meet.
- Focuses on consumer engagement, dignity, and quality of care.
- Strengthens compliance and accountability requirements for directors.
4. Risk Management: Identifying and Mitigating Risks
Effective risk management is essential for directors to meet their governance obligations. Aged care providers must have structured systems to identify, assess, and respond to risks.
Auditors will check:
- Whether risk registers are actively reviewed and updated.
- How incidents are reported, investigated, and addressed.
- Board meeting minutes to ensure directors are discussing risk and governance.
There are three key types of risk directors must be across:
Clinical and Care Risks
Refer to the Serious Incident Response Scheme (SIRS) and Draft Strengthened Quality Standards provider guidance material for Standard 5 for comprehensive details. In summary:
- Falls, medication errors, and inadequate clinical governance are significant concerns.
- Serious Incident Response Scheme (SIRS) data should be regularly reviewed.
- Staff competency assessments must be conducted to ensure proper clinical care.
Workforce and Safety Risks
Workforce-related obligations are outlined in the strengthened Aged Care Quality Standards provider guidance material for Standard 2, and the mandatory care minute requirements. In summary:
- High staff turnover or understaffing can severely impact care quality.
- Directors must ensure safe staffing ratios and compliance with minimum care minute requirements.
Organisational and Financial Risks
Refer to corporate governance guidelines and financial prudence obligations outlined in the Aged Care Act 2024. In summary:
- Boards must oversee financial sustainability to ensure services remain viable.
- Directors should review budget allocations to prioritise quality and safety.
5. Resourcing and Responsiveness: Ensuring High-quality Care
Aged care providers must ensure adequate resources are allocated to support quality care. Directors and executives must assess key areas of performance and planning to meet their governance obligations.
Audit Considerations:
Auditors will assess how well governance structures align with resourcing and responsiveness. In summary, they will consider:
- Are staffing levels appropriate?
- Is the organisation investing in service improvements?
- How effectively is consumer feedback incorporated into governance?
Workforce Planning
Aged care providers must comply with staffing requirements, including the 24/7 registered nurse (RN) mandate and minimum care minute regulations. The Australian Government mandates that residential aged care providers must have at least one registered nurse on-site at all times to enhance the quality and safety of care.
Additionally, care providers must meet the 2025 minimum care minute requirement, ensuring residents receive adequate direct care each day. These policies are crucial in reducing workforce burnout, improving patient outcomes, and maintaining accreditation.
Resources to Support Workforce Planning
For official guidance on these workforce planning regulations, visit the Department of Health and Aged Care, 24/7 Registered Nurses Requirement.
View Ausmed’s Workforce Planning in Aged Care Guide.
Financial Resourcing
Leadership and operations teams must consider how financial decisions affect care outcomes. In summary:
- Budgets must prioritise care quality over financial gains.
- Funding allocations should support continuous service improvement.
Consumer Feedback and Complaints Handling
Effective feedback mechanisms are central to responsive care. In summary:
- Providers must have transparent processes for responding to feedback.
- Boards should review complaints data to identify systemic issues.
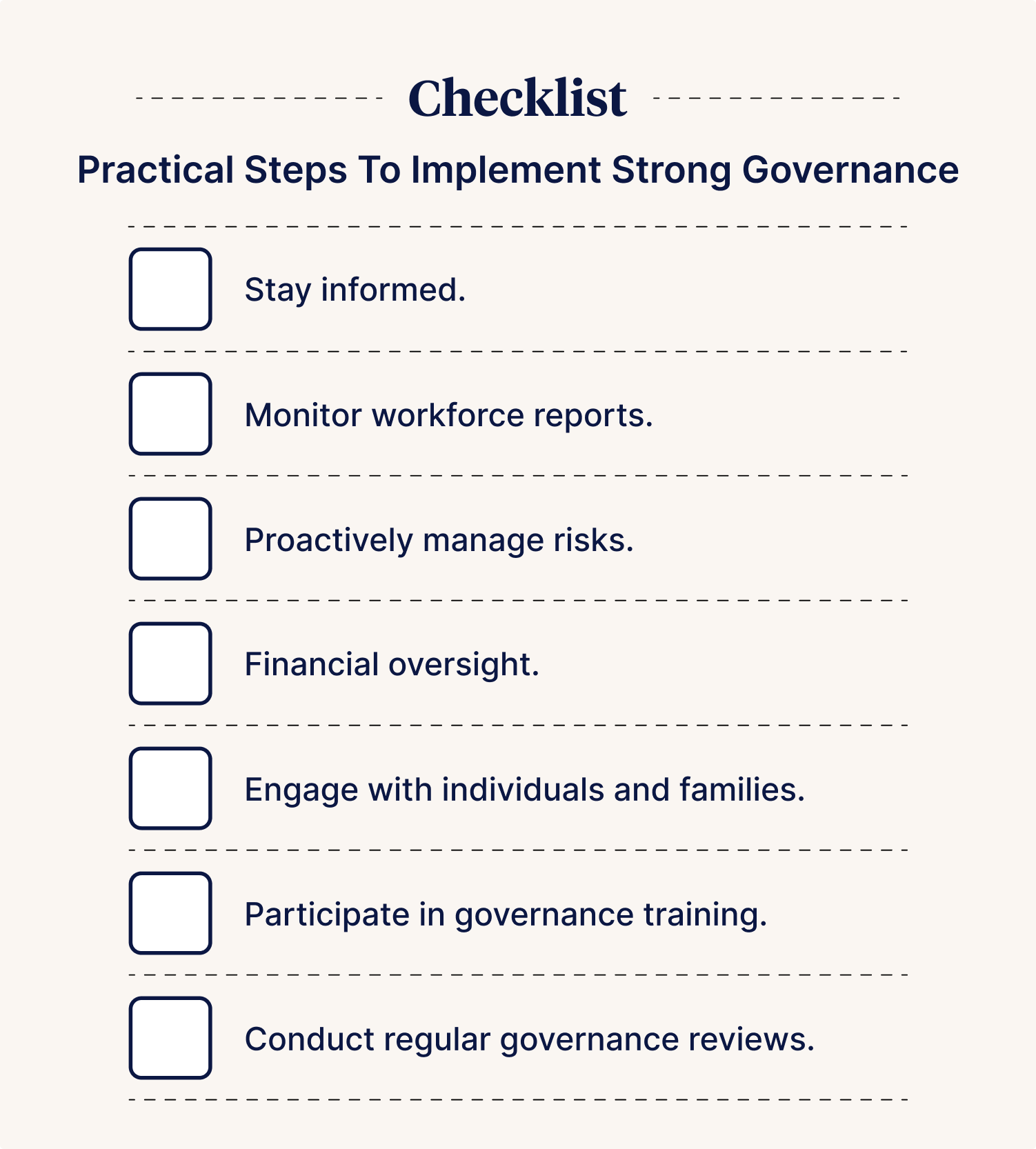
Checklist
To assist directors in meeting their governance obligations, the following checklist provides practical steps to implement strong governance:
- Stay informed. Review Aged Care Act 2024 updates, Code of Conduct changes, and workforce planning guidelines regularly.
- Monitor workforce reports. Ensure staffing levels comply with 24/7 RN mandates and that training programs are sufficient.
- Proactively manage risks. Maintain an active risk register, ensure timely incident reporting, and conduct safety audits.
- Financial oversight. Directors should prioritise care quality in budgeting decisions and ensure that funding allocations support workforce training and resident wellbeing.
- Engage with residents and families. Establish clear feedback mechanisms to ensure aged care services align with residents’ needs.
- Participate in governance training. Board members should complete ongoing CPD training on compliance, workforce planning, and aged care governance.
- Conduct regular governance reviews. Boards should schedule internal audits and governance assessments to identify gaps in compliance and service quality.
Learning from Other High-Risk Sectors: Governance Insights for Aged Care
Governance best practices in high-risk industries, such as banking, finance, and healthcare, offer valuable insights for aged care boards.
- Banking and finance: The Australian Prudential Regulation Authority (APRA) enforces strict governance standards to prevent misconduct. Aged care boards should adopt similar approaches, ensuring transparency, financial oversight, and accountability.
- Healthcare governance: Hospital boards oversee clinical safety, risk management, and patient outcomes. Aged care boards must take the same level of responsibility in ensuring resident safety and care quality.
- Corporate governance: Strong whistleblower protections and transparent decision-making help detect ethical violations and non-compliance, which are equally essential in aged care.
For comparisons between aged care and other high-risk industries, visit:
- APRA - Corporate governance principles.
- AICD - Best practices in governance and risk.
- Anchor Excellence - Managing the prevalence of risk in aged care.
For governance resources tailored to aged care board directors, visit the Aged Care Quality and Safety Commission – Provider Governance Requirements.
Author
Sigrid Piktin
Sigrid Pitkin is a Nurse Practitioner and board member with expertise in clinical governance, research, and healthcare innovation. She brings strategic insight and governance leadership to her roles on Food is Free and Climbing QTs boards.
With a background in allergy research, rural healthcare, and nursing education, Sigrid has held leadership positions at Monash University, Monash Children’s Hospital, and Murdoch Children’s Research Institute. She is also a Clinical Governance Committee member at Eucalyptus and a graduate of the AICD Foundations of Directorship program.
Passionate about equity, evidence-based care, and system reform, Sigrid combines clinical expertise with governance acumen to drive meaningful change in healthcare.