Australia’s aged care system is at a crossroads. The reforms, including mandating more minimum care minutes, strengthening clinical governance, and increasing transparency, are long overdue.
But will they be enough?
Regulation alone won’t fix the sector's chronic understaffing. Aged care must be seen as a place for skilled, multidisciplinary care, not just as a system that provides the bare minimum. The reforms are a step forward, but without investment in people across the entire workforce, they risk becoming another box-ticking exercise rather than a true transformation of care.
This piece contends that while government initiatives and wage increases are steps in the right direction, lasting change will require a fundamental shift in how aged care work and it’s workers, are valued, supported, and structured.
The Challenge of Workforce Sustainability
The Australian aged care sector faces a critical workforce shortage driven by an ageing population, increasing complexity of care needs, and workforce retention challenges. The introduction of the Strengthened Aged Care Quality Standards (February 2025) renews the focus on ensuring that aged care services are safe, effective, and person-centred.
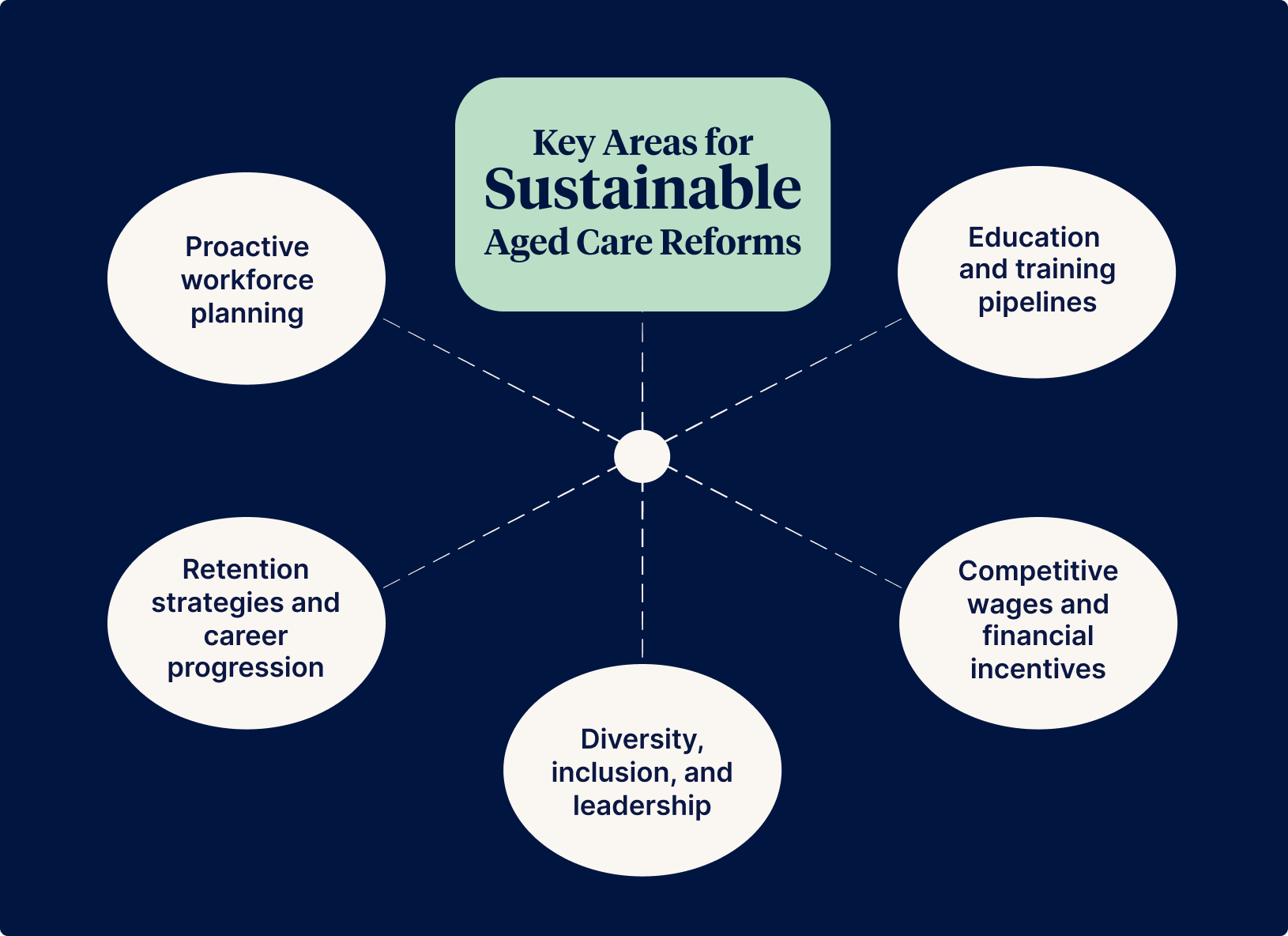
Key Areas for Sustainable Aged Care Reforms
I believe that aged care reforms will only be successful if a strong and sustainable workforce accompanies them. The following five key areas must be addressed if the reforms are to deliver the change we need:
- Proactive workforce planning
- Education and training pipelines
- Retention strategies and career progression
- Competitive wages and financial incentives
- Diversity, inclusion, and leadership
1. Workforce Planning: Moving from Reactive to Proactive
One of the major barriers to workforce sustainability within the aged care sector is the reactive approach to workforce planning. Many providers struggle with:
- Staff shortages and high turnover
- Lack of succession planning
- Inconsistent workforce distribution, especially in rural and regional areas
The strengthened standards now require aged care organisations to take a more proactive approach by:
- Identifying future workforce needs, particularly in specialist areas such as dementia and palliative care
- Developing structured training pipelines to ensure job-ready staff
- Prioritising direct employment models over casual or agency-based roles for greater job security
2. Education and Training: Investing in Future Skills
The government has introduced several scholarship programs to support nurses, nurse practitioners, and allied health professionals in aged care. These include:
- Aged Care Nursing Scholarship Program
- Primary Care Nursing and Midwifery Scholarship Program
- Aged Care Transition to Practice Program
- Dementia-related training for allied health professionals
These initiatives aim to enhance workforce skills and ensure high-quality, person-centred care. However, more must be done to support rural and regional workforce development through tailored training programs and incentives.
3. Retention: Creating Supportive and Sustainable Workplaces
Retention is just as important as recruitment. Many aged care workers leave the sector due to:
- Burnout and workplace stress
- Lack of career progression
- Heavy workloads and limited professional development opportunities
To improve retention, providers must focus on:
- Psychological safety and workplace culture – fostering supportive environments where staff feel valued
- Mental health support – offering structured mentoring programs and access to counselling
- Career pathways – providing competency-based training and study support for ongoing education
- Workload management – ensuring safe staffing ratios and realistic expectations
4. Pay and Financial Incentives: Addressing Workforce Drain
Pay remains one of the most significant barriers to workforce attraction and retention. While the Fair Work Commission wage increase was positive, aged care salaries still lag behind hospital-based roles. This has led to an ongoing workforce drain, with many professionals moving to higher-paying sectors.
To address this issue:
- Government investment is needed to sustain wage growth
- Aged care funding models should be reviewed to allow for competitive salaries
- Salary packaging, retention incentives, and bonus schemes should be explored
5. Diversity, Inclusion, and Leadership: Strengthening the Workforce
A diverse aged care workforce improves care quality and ensures services meet the needs of Australia’s multicultural and First Nations communities. Key strategies include:
- Encouraging young workers – through traineeships and school-based programs
- Improving visa pathways – to attract skilled migrant workers
- Recruiting First Nations carers – to provide culturally appropriate care
- Supporting older workers – through flexible roles and transition programs
Leadership and governance are crucial to workforce sustainability. Aged care organisations must:
- Demonstrate accountability for workforce wellbeing and quality care
- Engage staff in decision-making and ensure transparency in recruitment and training policies
- Develop leaders who understand frontline challenges and foster a positive workplace culture
The Future of Aged Care Workforce Reforms
The strengthened Aged Care Quality Standards set a new benchmark for Australian aged care. However, their success depends on attracting and retaining a quality workforce. To achieve this, aged care work must be recognised as a skilled profession that is:
- Respected and valued
- Well-paid and financially secure
- Built for long-term sustainability
If these reforms are implemented effectively, Australia has the opportunity to create an aged care system that not only meets regulatory requirements but also becomes a leading example globally of workforce excellence. The future of aged care depends on our commitment to investing in its people.
Further Reading
Want to learn more? For more insights on workforce sustainability, check out these recent guides:
Ensure your organisation is prepared for your first audit under the strengthened Standards.
Author
Sigrid Piktin
Sigrid Pitkin is a Nurse Practitioner and board member with expertise in clinical governance, research, and healthcare innovation. She brings strategic insight and governance leadership to her roles on Food is Free and Climbing QTs boards.
With a background in allergy research, rural healthcare, and nursing education, Sigrid has held leadership positions at Monash University, Monash Children’s Hospital, and Murdoch Children’s Research Institute. She is also a Clinical Governance Committee member at Eucalyptus and a graduate of the AICD Foundations of Directorship program.
Passionate about equity, evidence-based care, and system reform, Sigrid combines clinical expertise with governance acumen to drive meaningful change in healthcare.