How Minor Deviations Become Systemic Issues
Good Intentions
The path to non-compliance is rarely a dramatic plunge into chaos. It is often paved with good intentions. Shortcuts, workarounds, or quick fixes made in the name of efficiency. These can lead to a gradual erosion of standards. This "incremental decline" itself may even become normalised over time, further exacerbating the situation. The result is potentially poorer outcomes for health consumers, or to use ‘sector nomenclature’ … clinical and organisational risk, an inexperienced workforce, lower compliance, cost and service viability implications, and potential harm.
This thought leadership piece examines how minor deviations become systemic issues, challenging the normalisation of poor care before it takes hold. We will explore how workforce pressures, precisely the experience-complexity gap, exacerbate this decline before offering a compelling case for why building workforce capability is a timely strategy to address these challenges.
Some of the factors we will explore relate to organisational decision-making, but some do not. In fact, it’s the environmental, micro-economic, societal attitudes and population changes that will be the larger area of our focus. These indirect factors are often overlooked because they are essentially ‘out of our control’, yet understanding them is critical to the solutions we design and implement. This is the difference between systematic thinking and a reactive or haphazard approach, where you respond to variables rather than the structural flaw of the thing itself.
Subtle Signs of Slippage
Non-compliance rarely begins with overt negligence. Instead, it emerges subtly through repeated minor deviations from best practices.
For example:
- Overworked staff cut corners under the guise of "just this once."
- There is a subtle cultural drift from best practices to workplace norms, where "good enough" becomes “the way we’ve always done it.”
- Leaders who unknowingly deprioritise excellence in favour of immediate operational budget balancing.
- Education and learning teams obsess over maintaining essential compliance and forget the impact of building competence and confidence in the workforce.
Over time, these factors intertwine and compound, eroding the systems, processes, and cultures designed to provide excellence in care.
The Anatomy of Incremental Decline
These deviations can stem from genuine and present factors we see daily in health and aged care. We commonly hear the issue described in platitudes. The terms “workforce pressures”, “workforce challenges”, or “workforce issues” are now firmly rooted in the modern vernacular of healthcare.
These terms have become somewhat clichés. We use the words “pressures,” “challenges,” and “issues” so much these days, I think we’ve forgotten what they mean! So, I will stop referring to them as “workforce challenges” and instead call a spade a spade.
Our issue is a decline in the experience of our workforce.
The Experience-Complexity Gap
In December 2019, Virkstis, Herleth, and Rewers wrote in the Journal of Nursing Administration that hospitals and health systems face a unique challenge within the nursing workforce: a shortage of experience. As experienced nurses retire and the number of new nurses entering rises, overall experience across the workforce is declining.
Simultaneously, care provision is growing increasingly complex.
This challenge is known as the "experience-complexity gap”. The authors stated that this gap will likely widen without intervention, jeopardising the quality of care and patient safety.
Then came COVID-19, which amplified all the factors discussed.

2024 Australian workforce data shows high exit rates among nurses and midwives.
Unintended Consequence of Success
Putting COVID-19 aside for now and acknowledging it exacerbated the experience-complexity gap, believe it or not, these “workforce pressures” also come from a place of good intention, even success. We have more demand for health care, aged care, home care, and disability care because more funding is allocated (yes, it’s not enough, but bear with me).
We have greater complexity of care needs, partly driven by complex chronic illnesses but also because medical technologies and advancements help people live longer. We have greater expectations of care from our recipients, patients, clients, and participants because we advocate that they receive that through regulatory mechanisms and legislation. We also have eased some of the shortfalls in attracting nurses.
These are all wins, right? We deliberately set out over the past 2 decades to achieve this, and we can celebrate! More people are receiving care, living longer, and advocating for the high-quality, rights-based, respectful, person-centred care they deserve.
So why aren’t we celebrating? Why do these ‘wins’ feel like huge issues to contend with?
Pinpointing the Issue
Even if the solution is not, the issue is simple: Our workforce experience is declining. We have a demand and supply problem:
- Greater demand for services.
- Increased complexity of care requirements.
- Higher expectations of quality care from consumers.
- Tighter regulatory requirements to maintain compliance with.
Compounding with:
- High exit rate of nurses.
- Greater inflow of novice and early-career staff.
- A decline in the average experience of staff.
- Staff who feel burnt out and worry they are ill-equipped to provide sufficient care - yet aren’t working to the full scope of their practice.
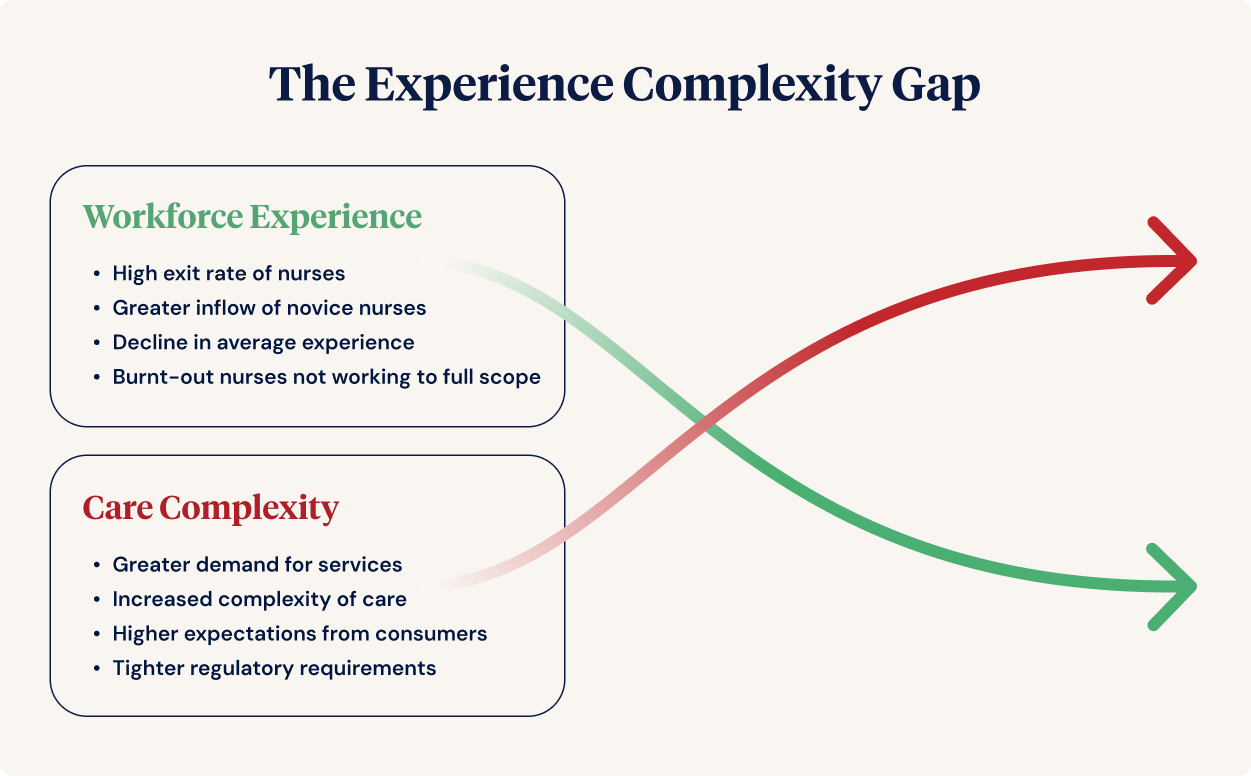
"Supply" and "Demand" issues contributing to the Experience-Complexity Gap.
Rejecting the Normalisation of Poor Care
Once deviations become routine, substandard practices become normal. This cultural shift manifests in several ways, notably the presence of high-impact, high-prevalent events.
A high-impact, high-prevalent event is a situation or incident that often occurs and has significant consequences for residents, staff, or the facility. If and when it happens, the severity of the clinical care risk makes a high impact.
Worryingly, a highly prevalent, high-impact event may be ‘normalised’ due to its frequency. Suppose staff new to the organisation and happen to be at the beginning of the novice-expert continuum (lacking experience) see an event such as a fall, incontinence-associated dermatitis, or a medication incident occurring constantly.
Clinical care risks are seen as inevitable, and deviance from practice is validated. Remaining in an environment where better practice options are reduced compounds this belief that clinical care risks are ‘normal’.
Combatting Incremental Decline
To stop this trajectory, leaders must boldly confront normalised poor care and acknowledge that even minor lapses have significant implications. The experienced leaders and clinicians who, if you’re lucky enough, still provide care and stewardship at your organisations will agree with me; the answer isn’t superficial; let me unpack it briefly.
Solutions lie in retaining experienced staff, providing targeted training, and offering robust support systems to mid-career staff. Accelerating the competence of novice nurses through team-based care and education models and strategically distributing clinical expertise within the organisation can make a significant difference. However, we need to carefully monitor the potential for preceptorship burnout from the experienced staff who are often required to foster emerging clinical leaders.
Building Workforce Capability
This bundled approach to alleviating the experience-complexity gap is simply building workforce capability. Our National Nursing Workforce Strategy calls for the active prioritisation and support of your staff's collective knowledge, skills, attitudes, and competencies, enabling nurses to work to the full scope of their practice. Ultimately, this drives your capacity to provide effective care and sustain organisational growth. For targeted initiatives, consider strategies to support mid-career staff and to foster emerging clinical leaders.
Building workforce capability acknowledges that the entire workforce needs support, growth opportunities, and enablement, not just our bright, young novices and early-career entrants. For example, experienced staff of 10+ years maintain their tenure because they feel valued and can transfer their knowledge to novice and early-career staff.
Ready to transform your approach to workforce capability?
Watch the Compliance Capability Webinar Series Now. Designed for educators, L&D professionals, HR teams, and anyone involved in staff induction, onboarding, and training.
We explore innovative ways to rethink the impact of education programs. Learn how to use insights to build a capable workforce and drive continuous improvement across your organisation.
References
Australian Government Department of Health and Aged Care 2024., National Nursing Workforce Strategy, viewed 30 October 2024, https://www.health.gov.au/our-work/national-nursing-workforce-strategy.
Australian Government Department of Health and Aged Care 2024., Unleashing the Potential of our Health Workforce: Scope of practice review, viewed 30 October 2024, https://www.health.gov.au/our-work/scope-of-practice-review.
Australian Health Practitioner Regulation Agency (Ahpra) 2022/23, Annual Report: Growing a safe workforce 2022/23, Ahpra, viewed 30 October 2024, https://www.ahpra.gov.au/Publications/Annual-reports/Annual-report-2023.aspx.
Braithwaite, J., Herkes, J., Ludlow, K., et al. 2017, 'Association between organisational and workplace cultures and patient outcomes: systematic review', BMJ Open, vol. 7, e017708, https://doi.org/10.1136/bmjopen-2017-017708.
Jarden, R.J., Jarden, A., Weiland, T.J., Taylor, G., Bujalka, H., Brockenshire, N. & Gerdtz, M.F. 2021, 'New graduate nurse wellbeing, work wellbeing and mental health: A quantitative systematic review', International Journal of Nursing Studies, vol. 121, 103997, https://doi.org/10.1016/j.ijnurstu.2021.103997.
Mazzetti, G. & Schaufeli, W.B. 2022, 'The impact of engaging leadership on employee engagement and team effectiveness: A longitudinal, multi-level study on the mediating role of personal- and team resources', PloS one, vol. 17, no. 6, e0269433, https://doi.org/10.1371/journal.pone.0269433.
McGillion, T. 2024., Building mid-career competence, viewed 25 November 2024, https://www.ausmed.com.au/organisations/toolbox/thought-leadership/building-mid-career-competence.
Rabin, S., Kika, N., Lamb, D., Murphy, D., Am Stevelink, S., Williamson, V., Wessely, S. & Greenberg, N. 2023, 'Moral Injuries in Healthcare Workers: What Causes Them and What to Do About Them?', Journal of Healthcare Leadership, vol. 15, pp. 153–160, https://doi.org/10.2147/JHL.S396659.
Virkstis, K., Herleth, A. & Rewers, L. 2019, 'Closing nursing's experience-complexity gap', The Journal of Nursing Administration, vol. 49, no. 12, pp. 580–582, https://doi.org/10.1097/NNA.0000000000000818.
Author
Zoe Youl
Zoe Youl is a Critical Care Registered Nurse with over ten years of experience at Ausmed, currently as Head of Community. With expertise in critical care nursing, clinical governance, education and nursing professional development, she has built an in-depth understanding of the educational and regulatory needs of the Australian healthcare sector.
As the Accredited Provider Program Director (AP-PD) of the Ausmed Education Learning Centre, she maintains and applies accreditation frameworks in software and education. In 2024, Zoe lead the Ausmed Education Learning Centre to achieve Accreditation with Distinction for the fourth consecutive cycle with the American Nurses Credentialing Center’s (ANCC) Commission on Accreditation. The AELC is the only Australian provider of nursing continuing professional development to receive this prestigious recognition.
Zoe holds a Master's in Nursing Management and Leadership, and her professional interests focus on evaluating the translation of continuing professional development into practice to improve learner and healthcare consumer outcomes. From 2019-2022, Zoe provided an international perspective to the workgroup established to publish the fourth edition of Nursing Professional Development Scope & Standards of Practice. Zoe was invited to be a peer reviewer for the 6th edition of the Core Curriculum for Nursing Professional Development.