Increased intracranial pressure is a medical emergency with the potential for a variety of serious complications, including death. It requires urgent treatment (MedlinePlus 2023).
What is Increased Intracranial Pressure?

Increased intracranial pressure (ICP) occurs when pressure is elevated inside the cranial vault, which contains three components:
- The brain
- Cerebrospinal fluid (CSF)
- Blood.
(Pinto et al. 2023)
The cranial vault is often described using the Monro-Kellie doctrine - the hypothesis that the cranial vault is similar to a fixed box, where any change in the volume of its contents leads to an increase in pressure (Nickson 2024).
Using this hypothesis, the three components of the cranial vault can be considered to have a fixed total volume; therefore, if one of the three components (brain matter, cerebrospinal fluid or blood) increases in volume, there is little capacity for the total intracranial volume to increase. This results in raised intracranial pressure, which can have a variety of serious consequences (Pinto et al. 2023; AMBOSS 2023).
Typically, when a person is in the supine position, the pressure inside the cranial vault is at or below 15 millimetres of mercury (mmHg) in adults and lower in children. ICP adjusts when the head's position changes relative to the body and in response to physiological processes such as sneezing and coughing (AMBOSS 2023).
An ICP of 20 mmHg or more indicates pathologic intracranial hypertension (AMBOSS 2023).
Causes of Increased Intracranial Pressure
Factors that can increase the volume of the cranial vault, and consequently lead to raised ICP, include:
- Hydrocephalus - an increase in cerebrospinal fluid (e.g. caused by increased CSF production or a choroid plexus tumour)
- A decrease in the reabsorption of cerebrospinal fluid (e.g. caused by obstructive hydrocephalus or meningeal inflammation)
- Intracranial haemorrhage (bleeding) or haematoma
- Swelling in the brain
- Trauma to the head or brain
- Brain tumour or abscess
- Certain infections (encephalitis or meningitis)
- Intracranial hypertension (when idiopathic, often affects young, overweight females aged between 20 and 45 years)
- Stroke
- Increased venous pressure (e.g. caused by cardiac failure)
- Metabolic disturbances (e.g. hyponatraemia, hepatic encephalopathy)
- Epilepsy or seizures
- Artefact (object).
(Pinto et al. 2023; AMBOSS 2023; NORD 2020; Nickson 2024)
Signs and Symptoms of Increased Intracranial Pressure
The symptoms of increased ICP are known to be non-specific and might resemble other conditions (Carey & Zimlich 2023).
The most characteristic symptom of increased ICP is a severe, unbearably painful headache. It may awaken the patient at night and not be relieved by analgesic medicines (NORD 2020).
A headache indicative of increased ICP might also be exacerbated by moving the head or coughing and is often associated with an altered mental state (Willacy 2021).
Other potential symptoms of increased ICP include:
- Nausea and vomiting
- Altered mental state, e.g. irritability, impaired decision-making, abnormal social behaviour
- Vision changes, e.g. blurry vision, double vision, photophobia, papilloedema (swelling of the optic disc)
- Weakness and lethargy
- Pupillary changes, e.g. irregularity or dilatation in one eye
- Motor changes
- Seizures
- Hypertension
- Irregular respiration
- Bradycardia
- Widened pulse pressure (a wide gap between systolic and diastolic blood pressures)
- Slow, irregular pulse
- Macrocephaly, bulging fontanel and sunset eye sign (in infants).
(Pinto et al. 2023; Willacy 2021; AMBOSS 2023; Carey & Zimlich 2023)
Cushing’s Triad
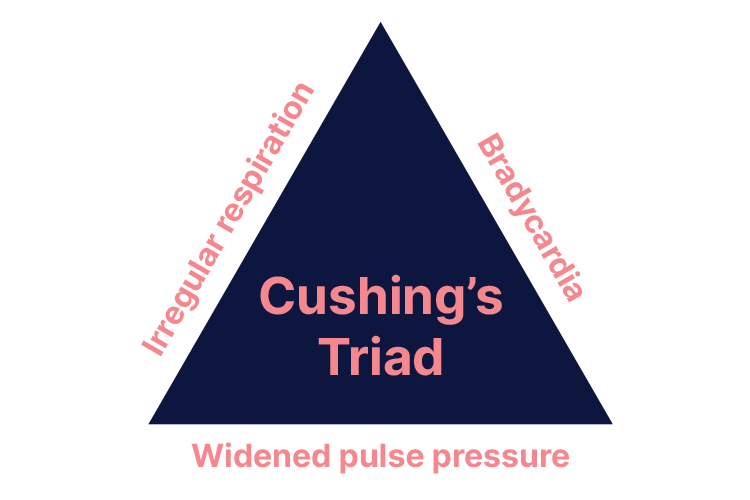
Cushing’s triad is a set of three clinical signs indicative of increased ICP. These signs are:
- Bradycardia
- Irregular respiration
- Widened pulse pressure.
(Mauldin 2025)
Cushing’s triad occurs when increased ICP significantly decreases cerebral blood flow, increasing arterial pressure to overcome the increased ICP (Dinallo & Waseem 2023).
At this point, if treatment does not occur to stabilise the ICP, herniation of the brain stem and occlusion of the cerebral blood flow can occur, with dire consequences (Dinallo & Waseem 2023).
Complications of Increased Intracranial Pressure
Potential complications of increased ICP include:
- Coma
- Optic atrophy
- Seizures
- Neurological damage
- Brain herniation, which is potentially fatal and is preceded by Cushing’s triad
- Death.
(Pinto et al. 2023; Willacy 2021; Cleveland Clinic 2024)
Diagnosing Increased Intracranial Pressure
Increased ICP may be diagnosed using:
- Medical history and physical examination, including a neurological exam
- Lumbar puncture (spinal tap) to measure the pressure of the cerebrospinal fluid
- CT scan
- MRI scan
- Funduscopic exam to assess for papilloedema (swelling of the optic discs), which is indicative of ICP.
(Cleveland Clinic 2024)
As a general rule, any patient presenting with a headache, vomiting and blurred vision should undergo head imaging to rule out increased ICP. Furthermore, those who have experienced a severe traumatic brain injury presenting with a Glasgow Coma Scale score of 3 to 8 should undergo ICP monitoring in accordance with severe traumatic brain injury management guidelines (Pinto et al. 2023).
Management of Increased Intracranial Pressure
The main principles of managing increased ICP should be:
- Raising mean arterial pressure in order to maintain cerebral perfusion pressure
- Addressing the underlying cause
- Lowering the ICP
- Preventing secondary injury.
(Pinto et al. 2023; AMBOSS 2023)
Note: Always ensure ICP readings are correct and rule out measurement errors (Nickson 2024). Always adhere to your local guidelines.
If the patient requires acute resuscitation and stabilisation, always follow the ABCDE assessment approach and ensure airway management, ventilation and circulation are prioritised (Pinto et al. 2022; AMBOSS 2022).
Once the patient is stabilised, management of increased ICP in the critically ill patient in an intensive care environment might include:
- Removal of any artefacts causing the raised ICP
- Maintaining adequate oxygen delivery
- Maintaining adequate cerebral perfusion pressure (CPP = MAP – ICP) using fluid, inotropes and vasopressors
- Elevating the head of the bed to optimise the venous return from the brain
- Avoiding cerebral vasoconstriction by monitoring PaCO2 levels
- Decreasing cerebral metabolic rate (the amount of oxygen and glucose the brain needs) - this may be achieved through sedation, analgesia, paralysis, avoiding hyperthermia, treating seizures, and barbiturate (induced) coma
- Administering osmotherapies such as mannitol or hypertonic saline to reduce intracranial pressure (to draw oedema out of the cerebral tissues to decrease ICP)
- Considering hypothermia (in some situations, only with the goal of reducing cerebral metabolism)
- Surgical techniques such as insertion of an extraventricular drain (EVD), evacuation of haematoma and/or decompressive craniotomy. (It’s important to note that decompressive craniotomy remains contentious following the DECRA trial. More on this topic can be found here.)
(Nickson 2024)
Note: A study by Monash University (n.d.) discourages the use of albumin in the resuscitation of critically ill patients with a traumatic brain injury, as it may increase the risk of mortality. Always adhere to your local guidelines.
Remember:
- Any changes in the volume of the cranial vault (blood, CSF or brain tissue) lead to an increase in pressure
- Any patient presenting with a headache, vomiting and blurred vision should undergo head imaging to rule out increased ICP
- Cushing’s triad is a set of three clinical signs indicative of increased ICP
- Increased intracranial pressure is a medical emergency with the potential for a variety of serious complications, including death.
Test Your Knowledge
Question 1 of 3
What is the typical intracranial pressure in adults?
Topics
References
- AMBOSS 2023, Elevated Intracranial Pressure and Brain Herniation, AMBOSS, viewed 1 July 2025, https://www.amboss.com/us/knowledge/elevated-intracranial-pressure-and-brain-herniation/
- Cleveland Clinic 2024, Increased Intracranial Pressure (ICP), Cleveland Clinic, viewed 1 July 2025, https://my.clevelandclinic.org/health/diseases/increased-intracranial-pressure-icp
- Carey, E & Zimlich, R 2023, ‘Understanding Increased Intracranial Pressure’, Healthline, 20 April, viewed 1 July 2025, https://www.healthline.com/health/increased-intracranial-pressure
- Dinallo, S & Waseem, M 2023, ‘Cushing Reflex’, StatPearls, viewed 1 July 2025, https://www.ncbi.nlm.nih.gov/books/NBK549801/
- Mauldin, A 2025, Cushing’s Triad, Osmosis, viewed 1 July 2025, https://www.osmosis.org/answers/cushings-triad
- MedlinePlus 2023, Increased Intracranial Pressure, U.S. Department of Health and Human Services, viewed 1 July 2025, https://medlineplus.gov/ency/article/000793.htm
- Monash University n.d., SAFE-TBI and SAFE-TBI II, Monash University, viewed 1 July 2025, https://www.monash.edu/medicine/sphpm/anzicrc/research/safe-tbi-ii
- National Organization for Rare Disorders 2020, Idiopathic Intracranial Hypertension, NORD, viewed 1 July 2025, https://rarediseases.org/rare-diseases/idiopathic-intracranial-hypertension/
- Nickson, C 2024, Increased Intracranial Pressure in TBI, Life in the Fast Lane, viewed 1 July 2025, https://litfl.com/increased-intracranial-pressure-in-tbi/
- Pinto, VL, Tadi, P & Adeyinka, A 2023, ‘Increased Intracranial Pressure’, StatPearls, viewed 1 July 2025, https://www.ncbi.nlm.nih.gov/books/NBK482119/
- Willacy, H 2021, Raised Intracranial Pressure, Patient, viewed 1 July 2025, https://patient.info/doctor/raised-intracranial-pressure
 New
New